Ready Reckoner for Medical Officers / General Practitioners
Ready Reckoner for Medical Officers / General Practitioners
- Side effects associated with anti-TB drugs and their prevention and management
- ADRs with anti-TB drugs, their prevention and management
- Laboratory test for TB patients
- Warning Symptoms for some serious adverse reactions
- Absolute contraindications of anti-TB drugs: (Benefit - Risk have to be carefully assessed)
- Algorithm for reintroduction of anti-TB drugs -To be done by experts only
- Stepwise increase in the dosage for Reintroduction
- Anti-TB drugs in pregnant & lactating women
- Contraception
- Anti-TB drugs in renally impaired patients
- Commonly used ancillary medicines
Side effects associated with anti-TB drugs and their prevention and management
Important general instructions
- Ensure that patient completes full course of anti-TB therapy
- Side effects of anti-TB drugs can be an important cause of patient stopping medication, especially with second line drugs
- Prevention and early detection of side effects are needed
- Alcohol, smoking and use of illicit drugs increase side effects
- Relevant history, clinical examination and lab tests are important to evaluate risk factors and diagnosis of side effects at an early stage
- For contraception, ask patient to seek advice from family planning center as oral contraceptives are less effective with some anti-TB drugs
- Educate, counsel and reassure patients for self-limiting side effects
- For side effects and serious side effects, take immediate action and refer patients to specialist as suggested below
- Report serious side effects to PvPI center (Procedure for reporting: Call your nearby PvPI center and provide complete information about side effect. (National toll free number: 18001803024)
- Advice nutritious diet to TB patients
- Advice patients about respiratory hygiene and provide information on preventing spread of TB (Cover nose and mouth with facemask, tissue paper)
ADRs with anti-TB drugs, their prevention and management
| ADRs | Diagnosis | Suspect Drug(s) | Differential Diagnosis/Other causes | Prevention | Management |
|---|---|---|---|---|---|
| Nausea and Vomiting | Clinical, based on complaints by patient | All oral anti-TB drugs | Hepatitis | Take anti-TB medication with banana | Symptomatic management.Exclude hepatitis / hepatoxicity |
| Rash, urticaria | Clinical | All anti-TB drugs | Steven Johnson syndrome, Anaphylactic reaction, Exfoliative dermatitis, Herpes infection | Seek past history allergy before starting treatment and as applicable | If rash involves <10% body drugs surface area (BSA) and is not with mucous membrane involvement, treat with anti-histaminics. Stop suspect anti-TB drug and refer patient to specialist if indicated. Desensitization can be attempted. If it fails, substitute the suspect drug with alternate drug |
| Diarrhea | Clinical | All oral anti-TB drugs | Bacterial dysentery,Amoebic dysentery, Malabsorption syndrome, Pseudomembranous colitis | Use of clean and potable water for drinking, washing hands before eating and drinking any thing | Advice Oral Rehydration Solution (ORS) 200 ml, after each loose stool. Check for any infective causes. |
| Liver enzymes- SGOT/SGPT (AST/ ALT) increased (up to 2xULN) | Increase of liver enzymes after starting anti-TB drugs | Frequent & Severe: PZA, INH, RIF Rare: EMB, Ethionamide, Fqs, PAS, Cycloserine |
Viral hepatitis-rule out by negative serological tests for A,B,C and E Alcoholic hepatitis- AST:ALT>2:1 with history of alcoho intak Amoebic liver abscess- Ultrasound/CT to detect cystic lesions /abscess Mass in ultrasound/CT -> Liver biopsy to rule out Hepatoma |
Up to 2xULN is not serious. Drug induced hepatitis is reported in 8-30 of patients. Avoid simultaneous administration of other hepatotoxic drugs It can worsen to severe hepatitis, which can be prevented by monitoring of LFT in high risk patients every 15 days & taking appropriate action if liver enzymes increase. |
Usually drugs are not withdrawn. Check for other potential hepatotoxic agents e.g alcohol |
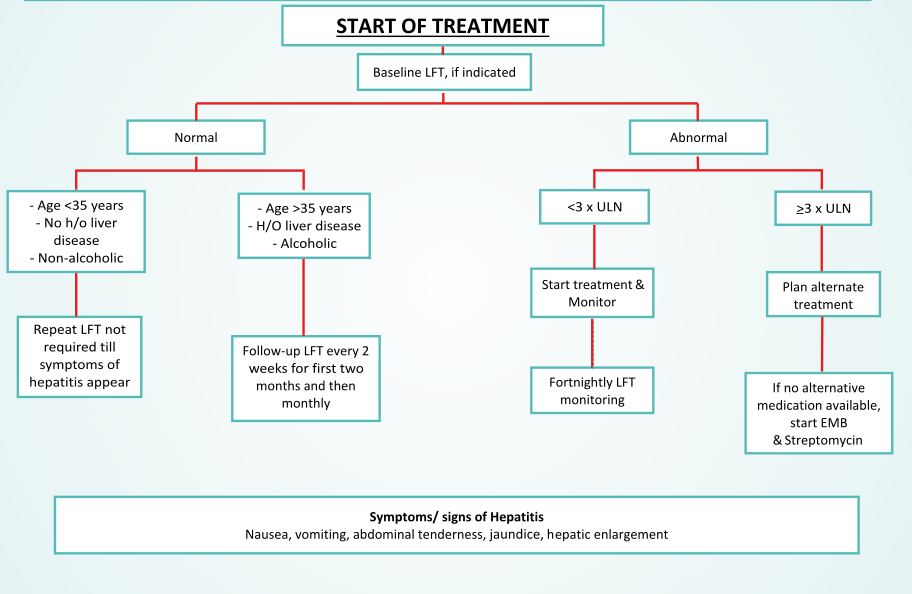
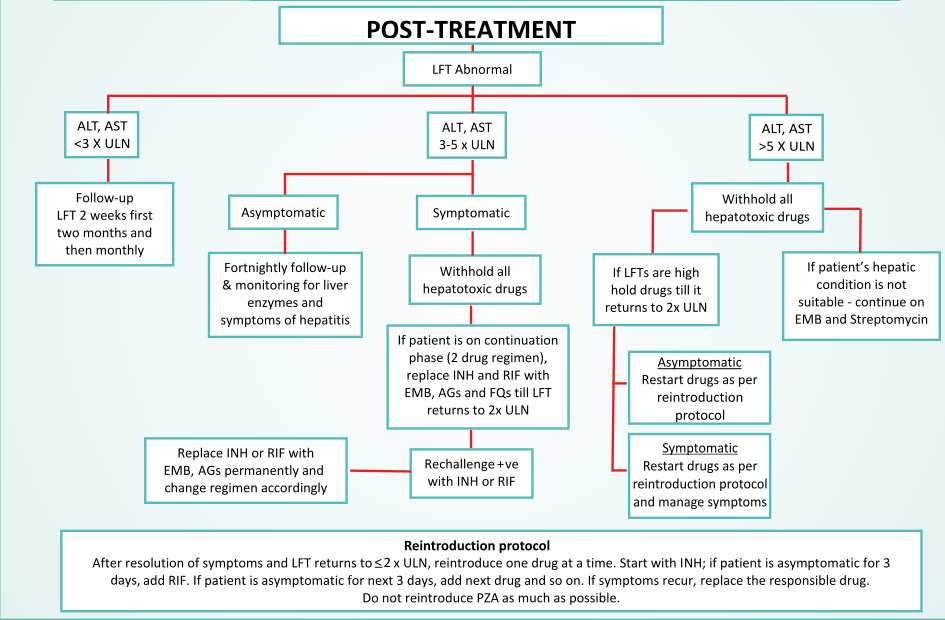
| Hepatitis(Severe) | ALT/AST > 3x ULN with symptoms of Nausea, vomiting, anorexia, jaundice, dark colored urine OR ALT/AST > 5xULN without symptoms | Frequent & Severe: PZA, INH, RIF Rare: Ethionamide, PAS, Cycloserine Clarithromycin Clofazimine Imipenemcilastatin | Investigate as above to rule out: Viral hepatitis, Alcoholic hepatitis, Amoebic liver abscess, Hepatoma | Early detection of raised liver enzymes to prevent worsening & reduce associated morbidity & mortality | Management includes withdrawal of potential causative drugs & supportive treatment.Later,when enzymes level return to normal, then gradually reintroduce the drugs (Refer to flowchart) |
| Exfoliative and allergic dermatitis | Clinical based on symptoms- Pruritus, widespread erythema and epidermal sloughing | Frequent : FAQ Rare: RIF, PAS Cycloserine linezolid Amoxicillin clavulanate clarithromicin Clofazimine | Asteatotic Eczema, Contact Dermatitis,Drug-Induced Bullous , Disorders, Drug-Induced Photosensitivity, Nummular Dermatitis, Perioral Dermatitis,Phytophotodermatitis | Early detection and management can prevent worsening antihistamines | Topical hydrocortisone or oral may be helpful to Pruritus, Anti-TB widespread RIF medications should not be discontinued unless an equally effective drug is available for substitution.Refer to specialist if indicated |
| Stevens-Johnson and Toxic epidermal necrosis | Clinical based on total body surface area (BSA) involvement of more than 10% and/or mucous membrane involvement | Rare: INH, RIF, EMB, Fqs, Amoxicillin-clavulanate clarithromycine imipenem-cilastatin | Staphylococcal scalded skin syndrome, Irradiation-History of radiation, Trauma-History, Progressive systemic sclerosis - ANCA antibodies. | Early detection and management can prevent worsening | Immediate drug withdrawal and referral to specialist is recommended. Supportive therapy like antihistamines, anti-inflammatory agents may be helpful in the meantime |
| Psychosis (Severe) | Symptoms of Hallucinations, paranoia, suicidal or abnormal thoughts or actions | Frequent & Severe: Cycloserine Frequent: INH Rare: RIF, FQs Clarithromycin Clofazimine Imipenem-cilastatin | Post-traumatic Stress Disorder, Delusional disorder, Schizophrenia, Schizophreniform Disorder | Careful monitoring. Psychiatric counseling at the start of treatment in patients at risk of psychiatric disorders. | Refer to specialist for further evaluation Consider suspect drug withdrawal. Refer to specialist |
| Peripheral neuropathy | Clinical symptoms of Burning and paresthesia in extremities. Electromyography (nerve conduction studies) for confirmation | Frequent: INH Rare:EMB, FQs, PAS, Ethionamide Cycloserine Linezolid (severe) |
Neuropathy due to high dose of pyridoxine Diabetic neuropathy Peripheral demyelinating disease | Supplementing the anti- TB drugs with Pyridoxine 5-10 mg orally once a day while patient is on INH Pyridoxine 50 mg per day with Linezolid and with every 250 mg Cycloserine | Check for Pyridoxine compliance. Give paracetamol / NSAIDs to alleviate pain. Drug withdrawal is not indicated. Start Pyridoxine 100 mg per day. If no response, increase dose of Pyridoxine to 200 mg. Refer to specialist if no response or if patient is taking Linezolid. |
| Ototoxicity/ Hearing loss/Deafness | Symptoms- Tinnitus, vertigo, Loss of balance and equilibrium. Audiometry for confirmation | Frequent & Severe: AGs Rare:Linezolid clarithromycin imipenem-cilastatin | Ear wax, otitis media, Traumatic hearing loss, Meniere's disease Acoustic neuroma | Monitoring of early symptoms can prevent permanent ear damage | Consider withdrawal of the suspect drug. Refer to specialist for further evaluation |
| Optic neuritis | Vision loss, Peri- ocular pain, Dyschromatopsia (disorder of color vision), based on symptoms and ophthalmic examination for confirmation | Frequent & Severe: EMB Rare: PAS Ethionamide Clofazimine Linezolid | Brain Tumor, Giant cell arteritis, Retinal detachment, Multiple sclerosis, Closed-angle glaucoma, Cataract, Macular degeneration, Diabetic retinopathy | Regular ophthalmologic examination | Consider withdrawal of the suspect drug. Refer to specialist for further evaluation |
| Immune Nephrotoxicity | Serum creatinine >2xbaseline. Presence of Auto- antibodies in the blood is confirmatory | RIF, especially when restarted after stopping for few weeks | Urinary tract infection, Post streptococcal glomerulonephritis, Minimal change disease, Rapidly progressing glomerulonephritis | Patients should be counseled not to stop and restart rifampicin randomly, on their own | Consider drug withdrawal and refer to specialist |
| Flu Syndrome | By symptoms- Chills, malaise, dry cough, shortness of breath, loss of appetite, body aches and nausea | Frequent: RIF - Specially with alternate day regimen | Viral infections: Influenza, Dengue Fever: Dengue NS1 antigen test positive | Patients on daily regimen have reported lower frequency and less severe flu as compared to the patients on intermittent regimen | Oral antihistaminics and paracetamol, according to the symptoms |
| Arthralgia / Arthritis | Joint pain, swelling involving one or more joint. High uric acid levels, demonstration of tophi crystals in joint is confirmatory of Gout | Frequent & Severe: PZA Rare: EMB, INH | Osteoarthritis, Rheumatoid arthritis | Early diagnosis and management can prevent progression and can improve quality of life | Therapy with paracetamol / NSAIDs can be used for pain relief as needed / Colchicine can be given in gout. |
| Thrombocytopenia | Blood platelet count <50000 /mm3 indicates thrombocytopenia, Drug induced thrombecytopenia is diagnosed by excluding other causes of thrombocytopenia | Frequent & Severe: RIF, FQs Rare: INH, EMB, PZA, AGs, PAS, Ethionamide Cycloserine Amoxicillin- clavulanate -Clarithromycin Imipenemcilastatin Linezolid | Dengue hemorrhagic fever - Dengue NSl antigen test positive Malaria - Peripheral blood smear, malaria antigen test Liver Cirrhosis - Liver Biopsy Thrombotic Thrombocytopenic Purpura Blood picture showing thrombocytopenia and hemolytic anemia with clinical symptoms Acute Leukemia - Bone marrow examination | Patients should be advised not to skip the doses of anti-TB drugs as the incidence of drug- induced thrombocytopenia has been reported to be higher when the drug is not taken continuously Regular monitoring of platelet levels can facilitate early detection & thus, reduce the associated morbidity & mortality | Manage with platelet transfusion and consider withdrawal of suspect drug. It is important to remember that anti-TB drugs can cause thrombocytopenia. |
| Leucopenia |
Leucocyte count Iess than 2000/mm 3 Neutropenia : Absolute neutrophil count less than 1000/mm3 Routine blood counts |
Rare: INH, EMB, RIF, FQs, AGs, Ethionamide Linezolid Amoxicillin Clavulanate Clarithromycin Imipenem-cilastatin | Typhoid, malaria, dengue, Rickettsial infections, HIV, thyroid disorders., aplastic anemia, rheumatoid arthritis, vitamin BI2 or folate deficiency, mineral deficiencies of copper and zinc. Bone marrow diseases: Myelodysplastic syndrome, leukemia, Autoimmune disorders: SLE, Bone marrow damage or suppression Drug induced Leucopenia, Clozapine, Valproate, Lamotrigine,Interferons and Bupropion | Monitoring of the complete blood count as indicated, will help in early identification. Avoid simultaneous administration of other drugs that can cause leucopenia. |
If the total leucocyte count is <2000/ mm3 or absolute neutrophil count <1000/mm3. Refer the patient to specialist as this is serious. |
| Nephrotoxicity | Serum creation more the twice the baseline with symptoms of Oliguria, loss of appetite, General ill feeling and fatigue | Frequent & Severe: AGs Rare: Linezolid | Chronic renal failure, Alcoholic keteacidosis, Diabetic keteacidosis, Metabolic acidosis, Urinary tract infection | Dose adjustment in patients with pre- existing renal disease, monitoring of renal function as indicated | Dose adjustment in patients with pre-existing renal disease. In cases of lack of response consider drug withdrawal and refer to specialist. |
| Hyperglycemia | Fasting blood sugar more than 160 mg/dl with polydypsia, polyphagia, polyuria | Rare: RIF, INH FQs, Moxifloxacin Clofazimine | Uncontrolled diabetes mellitus, Impaired glucose tolerance | Regular Blood sugar monitoring in high risk patients can help in early detection. | Individualized diet, exercise, patient education and glucose-lowering therapies. |
| Hypoglycemia | Blood sugar less than 55 mg/dl with weakness, palpitation, loss of consciousness, seizures | Rare: INH Ethionamide Clarithromycin | Prolonged starvation, Overdose of insulin or oral hypoglycemic agents in diabetic patients | Regular Blood sugar monitoring in high risk patients for early detection | In case of severe hypoglycemia, withhold all hypoglycemic medications. Glucose to be given orally or I.V as appropriate. |
| Hypothyroidism | TSH level >10 mIU/L with tiredness, increased sensitivity to cold, weight gain, constipation, depression, lethargy | Rare: PAS Ethionamide Cycloserine | Hypothyroid Goitre - TSH levels high Myxoedema - Hashimotos thyroiditis - Anti-thyroid antibodies Riedels thyroiditis -Antibodies | Early diagnosis, followed by prompt treatment can help to prevent worsening. | All patients with TSH >10 mIU/L, whether symptomatic or not, should be started on Levothyroxine |
| Pseudomembrano us colitis | Watery diarrhoea with or without blood, associated with stomach cramps and high fever, stool examination | Frequent & Severe: Amoxicillin - clavulanate Clarithromycin Imipenem-cilastatin Linezolid Rare:RIF, FQs | Viral diarrhea, Bacterial diarrhea, Amoebic dysentery, Malabsorption syndrome - Chronic condition accompanied with weight loss | Judicious use of antibiotics, use of probiotics | Vancomycin and metronidazole are effective. Refer to specialist. Consider withdrawal of the suspect drug. |
| Gynaecomastia | Clinical symptoms and biopsy | Rare: INH, RIF Ethionamide | Lipomas, dermoid cysts, sebaceous cysts, ductal ectasia, hematomas, and fat necrosis FNAC will provide diagnosis | Resolves after stopping anti-TB drugs | Reassure patient and in severe cases, withdraw suspects drug. |
| Pellagra-like syndrome | Based on clinical symptoms of Dementia, Dermatitis and Diarrhea | Rare: INH Ethionamide | Chronic alcoholism - Malnutrition Amino acid imbalance - Hypoalbuminemia | Supplementation with nicotinamide and pyridoxine | Check for compliance. Increase the dose of nicotinamide and pyridoxine if required. |
| QT prolongation Torsade de pointes Arrhythmia | QTc ≥ 501 ms on at least two separate ECGs and /or arrhythmia on ECG | Rare: FQs Moxifloxacin Clofazimine Linezolid Clarithromycin | Hypokalemia, Metabolic acidosis, Atrial fibrillation, atrial flutter, ventricular arrhythmia, Paroxysmal supraventricular tachycardia | ECG of patients on FQs as and when indicated | Refer to specialist for management |
Pancreatitis, Peptic ulcer, Depression, Encephalopathy, Pneumonitis, Myopathy, Rhabdomyolysis, Congestive cardiac failure, Pericarditis have also been reported rarely with anti-TB drugs.
Peripheral neuropathy, anemia, thrombocytopenia and optic neuritis with Linezolid (2nd line drugs) can be severe and need immediate referral to specialist.
Frequent: Seen in 1-10% patients
Rare: Seen in less than 1% patients
Laboratory test for TB patients
| Timepoints | Laboratory tests |
|---|---|
| Baseline (Before initiating treatment if indicated) |
|
| After 1.5 months | Ophthalmologic examination (for patients taking Ethambutol), if indicated |
| After 2 months of treatment as indicated |
Tests mentioned at the baseline will be repeated Ophthalmologic examination: If EMB is stopped at or before 2 months, not required. If EMB is continued and ophthalmologic examination was not performed at 1.5 months, then it should be done. |
Tests to be performed at 2 months will be repeated at 4 and 6 months if indicated.
Warning Symptoms for some serious adverse reactions
| Warning Symptoms | For Medical officer/ General practitioner (GP): When to refer the patient |
|---|---|
|
Rash Skin lesions on oral cavity, nose |
If mucous membranes are involved OR rash is more than 10% of body surface area without mucous membrane involvement OR associated with fever and generalised swelling (edema); refer to specialist/tertiary care center immediately. |
| Pain in eye/s, Blurring of vision and Disturbance in color vision |
Indicates Eye toxicity Refer the patient to specialist for evaluation |
| Loss of hearing/ Diminished hearing, Ringing in the ears, Dizziness and Loss of balance | Indicates Ear toxicity Refer the patient to specialist for evaluation. |
| Puffiness of face, Swelling over feet and Oliguria Anuria | Indicates Kidney toxicity. Treat the symptoms and refer the patient to specialist for evaluation. |
| Hallucinations, Seeing abnormal things and Suicidal or abnormal thoughts or actions | Indicates Psychiatric disturbances. Refer the patient to specialist for evaluation. |
Absolute contraindications of anti-TB drugs: (Benefit - Risk have to be carefully assessed)
| Drug | Absolute contraindications | Reason |
|---|---|---|
| Rifampicin | With Saquinavir and Ritonavir | Potential for hepatotoxicity is increased. Rifampicin is CYP3A4 inducer and can decrease Saquinavir level and effect |
| Ethambutol | Optic neuritis | Ethambutol can cause optic neuritis |
| Pyrazinamide |
Acute porphyria Gouty arthritis |
Pyrazinamide can precipitate acute porphyria Can inhibit excretion of urates Can cause drug induced hepatitis |
| Neomycin Kanamycin, Tobramycin, Amikacin, Capreomycin, Streptomycin | Concurrent use of two aminoglycosides With potent diuretics e.g. Furosemide Soon after use of anesthetics and muscle relaxants | Can potentiate nephrotoxicity Can potentiate otoandcity Can result in respiratory paralysis |
| Levofloxacin, Ofloxacin, Moxifloxacin | History of tendon disorders | Associated with risk of tendinitis and tendon rupture |
| Ethionamide | Severe hepatic impairment | Risk of worsening |
| Cycloserine |
Epilepsy, Psychiatric illness - Depression, Severe anxiety, Psychosis , Severe renal insufficiency |
Can precipitate seizures Can lead to severe psychosis and depression Can lead to Cycloserine toxicity |
| Clarithromycin | With Pimozide, Astemizole With Lovastatin or Simvastatin Hypokalemia and in patients with prolonged QT interval | Risk of QT prolongation Can cause rhabdomyolysis Risk of further QT prolongation |
| Imipenem | With Valproic acid and Probenecid | Decrease in valproic acid concentration and Increase in plasma levels of imipenem |
| Linezolid | With Monoamine oxidases A or B inhibitors (e.g. phenelzine, isocarboxazid, selegiline, moclobemide) within two weeks | Risk of MAO inhibition leading to serotonin syndrome |
Algorithm for reintroduction of anti-TB drugs -To be done by experts only
| Adverse drug reaction | Advice on reintroduction |
|---|---|
| Hepatotoxicity | Reintroduction after liver enzyme returns to ≤ 2 X ULN |
| Ocular toxicity |
Main suspect drug is EMB Reintroduction of Ethambutol is not recommended |
| Immune mediated Nephritis | Main suspect drag is RIF Reintroduction with RIF is not recommended |
| Non serious cutaneous ADRs - no mucous membrane involvement or less than 10 Ye of BSA. | After withholding all drugs reintroduce one drug at a time |
| Serious Cutaneous adverse drug reactions - mucous membrane imrolvement or more than 10 'Vs of BSA. | Reintroduction is not recommended (applies for all anti-TB drugs). |
| Immune thrombocytopenia |
Main suspect drug is RIF Reintroduction with RIF is not recommended |
| Gynecomastia | Symptoms takes long time to resolve (4-12 month) hence usually reintroduction is not required |
| Aplastic Anemia |
Main suspect drug is INH Reintroduction with INH is not recommended |
| Nephrotoxiicity |
Main suspect drags are AGs. AGs can be reintroduced at low doses after the renal function returns to normal |
| Ototoxicity |
Main suspect drugs are AGs. Reintroduction of AGs is not recommended. |
| Cardiac arrhythmias including Torse de pointes (TdP) |
Main suspect drugs are FQs. Reintroduction with FQs is not recommended. |
| Diarrhea | Reintroduction is recommended with one drug at a time every fourth day, once diarrhea is resolved |
| Seizures | Main suspect drugs are FQs. Reintroduction with FQs is not recommended. |
| Psychosis | Main suspect drugs is cycloserine. Reintroduction with cycloserine can be done at low dose but if symptoms recur than completely discontinue the drug. |
Stepwise increase in the dosage for Reintroduction
1. Reintroduction of anti-TB drugs:
| Drug | Day1 | Day2 | Day3 |
|---|---|---|---|
| Isoniazid | 50mg | Full dose | Full dose |
| Rifampicin | 75mg | 300mg | Full dose |
| Pyrazinamide | 250mg | 1000mg | Full dose |
| Ethionamide/Prothionamide | 125mg | 250mg | Full dose |
| Fluoroquinolones | 50mg | 200mg-250mg | Full dose |
| Cyclosporine | 125mg | 250mg | Full dose |
| Ethambutol | 100mg | 500mg | Full dose |
| PAS | 1g | 4g | Full dose |
| Capreomycin | 125mg | 500mg | Full dose |
| Kanamycin | 125mg | 500mg | Full dose |
| Amikacin | 125mg | 500mg | Full dose |
If the test dose of any drug causes a reaction discontinue this drug, unless it is deemed essential to the regimen. If that is the case, desensitization can be considered.
2.Reintroduction of the drugs should be in hospitalized patients.
3. In patients with severe rash, dose increment should be slower than stated above.
4.For key drugs, Isoniazid, Rifampicin, Ethambutol, detailed desensitization protocol with very small dose and method of dosage preparation is available on the website - (http://www.who.int/topics/tuberculosis/en/)
Anti-TB drugs in pregnant & lactating women
Pregnancy
- All female patients in reproductive age-group should be tested for pregnancy during initial evaluation
- Generally pregnancy should be avoided in TB patients
- Aminoglycosides (streptomycin, kanamycin, amikacin) are contraindicated through pregnancy
- Ethionamide is contraindicated in first trimester of pregnancy
- Mother's malnutrition may affect the development of the foetus
- Continuation of pregnancy should be done in consultation with gynecologist / obstetrician
- Pregnant patients need to be monitored carefully both in relation to treatment and progress of the pregnancy
Lactation
Breast feeding should not be discouraged. The mother should be advised about cough hygiene measures such as covering the nose and mouth while breast feeding, coughing, sneezing or any act which can produce sputum droplets. Most of the anti-TB drugs cross into breast milk at low levels. However the doses of drugs that babies receive via breast milk are insufficient to treat or prevent TB in the infant. Mothers receiving INH and their breastfed infants should be supplemented with vitamin B6 (pyridoxine), recommended dose of Pyridoxine in infants is 5 mg/day
Contraception
Rifampicin decreases the efficacy of oral contraceptives by increasing their metabolism so the use of Oral Contraceptive Pill (OCP) is not recommended during TB treatment. As per the patient's choice and availability, one of the following methods are recommended:
- Double barrier method of contraception i.e. condom with spermicide (foam, gel, cream, or suppository), diaphragm (including occlusive cap or cervical/vault) with spermicide
- IUD
- Medroxyprogesterone acetate
- High dose estrogen OCP
Anti-TB drugs in renally impaired patients
Dose modification for anti-TB drugs: Severity of renal impairment is defined by creatinine clearance (CrCl) and renal impairment is considered as: mild (1.5-2 mg/dL serum creatinine), moderate (2-3 mg/dL serum creatinine) and severe (> 3 mg/dL serum creatinine).
Estimated creatinine clearance calculations:
Men: Weight (kg) X (140 - age) / 72 X serum creatinine (mg/di)
Women: 0.85 X Weight (kg) X (190 - age) / 72 X serum creatinine (mg/d1))
| Drug | Recommended dose and frequency for patients with CrCI < 30 ml/min or for patients receiving haemodialysis | Drug | Recommended dose and frequency for patients with CrCI < 30 ml/min or for patients receiving haemodialysis |
|---|---|---|---|
| Isoniazid | No adjustment necessary | Gatifloxacin | 400 mg three times a week |
| Rifampicin | No adjustment necessary | Cycloserine | 250 mg once daily, or 500 mg / dose three times per week |
| Pyrazinamide | 25-35 mg/kg per dose three times per week (not daily) | Prothionamide | No adjustment necessary |
| Ethambutol | 15-25 mg/kg per dose three times per week (not daily) | Ethionamide | No adjustment necessary |
| Streptomycin | 12-15 mg/kg per dose two or three times per week (not daily) | PAS | 4 g/dose, twice daily maximum dose |
| Capreomycm | 12-15 mg/kg per dose two or three times per week (not daily) | Linezolid | No adjustment necessary |
| Kanamycin | 12-15 mg/kg per dose two or three times per week (not daily) | Clofazimine | No adjustment necessary |
| Amikacin | 12-15 mg/kg per dose two or three times per week (not daily) | Ammoxicillin/clavulanate | For 10-30 ml/min dose 1000 mg as amoxicillin component BD; For CrCI <10 ml/min dose 1000 mg as amoxicillin component OD |
| Ofloxacin | 600-800 mg per dose three times per week (not daily ) | Imipenem / cilastin | For CrCl 20-40 ml/min dose 500 mg every 8 hours; For CrCI <20 ml/min dose 500 mg every 12 hr |
| Levofloxacin | 750-1000 mg per dose three times per week (not daily) | Meropenem | For CrCI 20-40 ml/ min dose 750 mg every 12hr; For CrCI <20 ml/min dose 500 mg every 12 hr |
| Moxifloxacin | No adjustment necessary | High dose isoniazid | Recommendations not available |
Commonly used ancillary medicines
Management of adverse reaction often requires use of ancillary medicines to reduce or lessen side effects. Below is list of indications and commonly used medicines for management of adverse reactions.
| Indication | Drugs |
|---|---|
| Nausea, vaunting, Stomach upset | Domeperidone, metoclopramide, prochlorperazine, promethazine, ondansetron |
| Heartburn, indigestion and acidity | H2-blockers (ranitidine etc.), proton pump inhibitors (omeprazole, pantoprazole etc) Antacid syrups and the antacids if prescribed should be taken at least 2 hours apart from anti-TB drugs |
| Oral candidiasis | Fluconazole, clotrimazole lozenges, nystatin suspension |
| Diarrhoea | ORS sachets |
| Prophylaxis of peripheral neuropathy of cycloserine and isoniazid | Pyridoxine (vitamin B6) |
| Musculoskeletal pain, Arthralgia, headaches | Give paracetamol / ibuprofen / aspirin / diclofenac. If caused by fluoroquinolones, refer to specialist immediarely. Tendonitis can progress to tendon rupture. |
| Cutaneous reactions, itching | Hydrocortisone cream, calamine lotion |
| Systemic hypersensitivity Reactions | Antihistamines (diphenhydramine, chlorpheniramine, dimenhydrinate) Systemic corticosteroids (prednisone, prednisolone, Dexamethasone) are reserved only for very severe reactions |
| Bronchospasm | Inhaled beta-agonists (salbutamol, albuterol, etc.), inhaled corticosteroids (beclomethasone, etc.) |
| Hypothyroidism | Levothyroxine |
| Electrolyte wasting | Potassium and magnesium replacement therapy (oral formulations) |
Source: ICMR book on Prevention and management of adverse reactions associated with Anti TB drugs
अंतिम बेर संशोधित : 2/12/2020
Janani Suraksha Yojana (JSY) is a safe motherhood ...
This topic explains factors and variuos methods of...
Puerperium is the period after childbirth up to 6 ...
Provides information about Yoga for pregnant women
